What is a Total Hip Replacement?
A total hip replacement (THR) is an operation that replaces the worn-out ball and socket of the hip joint with artificial components. It is one of the most successful procedures in modern medicine, offering long-lasting pain relief and improved mobility for patients living with hip arthritis.
Treatment for total hip replacement includes optimisation before surgery, the operation itself, and post-operative care, all of which are explained here.
Why consider a total hip replacement?
A hip replacement is offered when:
- Pain is significantly limiting daily activities
- Non-surgical treatments (physiotherapy, injections, medication) are no longer effective
- Sleep, walking distance or ability to work are affected
- X-rays show moderate to severe arthritis
- The hip has become stiff, unstable or deformed
The goal of treatment is simple: less pain, better function, and improved quality of life.
Pre-operative Treatments & Preparation
Before surgery, several steps help ensure you are safe, prepared and able to recover quickly.
→ Physiotherapy
→ Activity modification
→ Weight optimisation (if needed)
→ A walking stick or other support
These measures help maintain mobility and strength before the operation.
→ Review medical history
→ Check blood tests, ECG and other investigations
→ Discuss anaesthetic options (spinal, general or combined)
→ Ensure your overall health is optimised
Exercises may include:
→ Gluteal strengthening
→ Core stability
→ Gentle range-of-movement exercises
Treatment During Surgery: What Happens in a Total Hip Replacement?
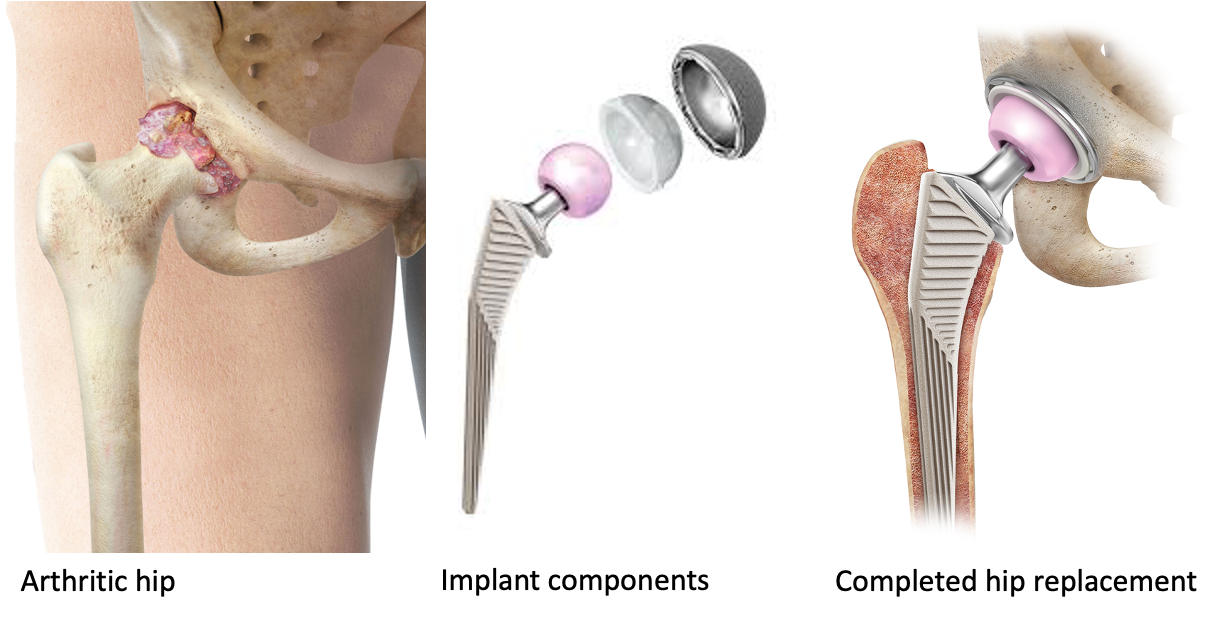
→ The arthritic femoral head (the ball at the top of the thigh bone)
→ The damaged cartilage lining the hip socket (acetabulum)
This removes the painful, worn surfaces responsible for stiffness and discomfort.
→ A metal acetabular cup is then inserted into the pelvis to recreate a smooth socket.
→ A liner (plastic, ceramic, or metal) is placed inside the cup to allow smooth, low-friction movement.
→ Acetabular cup – a metal shell fixed into the hip socket
→ Liner – typically polyethylene (plastic), ceramic, or metal
→ Femoral stem – a metal implant placed inside the thigh bone
→ Femoral head – a ball (ceramic or metal) that fits onto the stem
Fixation may be cemented or uncemented, depending on bone quality, patient factors, and surgeon preference.
→ A stable joint with low risk of dislocation
→ Correct leg length
Removing the Damaged Bone
01
The worn ball (femoral head) is removed and the socket is cleaned of arthritic bone.
Preparing the Bone
04
The pelvic socket is shaped and prepared to accept the replacement cup. The thigh bone is prepared for the stem.
Inserting Implants
02
A typical hip replacement consists of:
- Cup (acetabular component) – fits into the pelvis
- Liner – a smooth bearing surface
- Stem (femoral component) – fits into the thigh bone
- Ball (femoral head) – fits onto the stem
Implants can be:
- Cemented
- Uncemented
- Hybrid (one cemented, one uncemented)
- Your implant choice will be based on bone quality, anatomy, age and activity goals.
Checking Leg Length and Stability
03
The hip is tested to ensure stability, correct positioning and equal leg length.
Closing the Wound
05
The layers are closed, usually with dissolvable sutures, and a dressing is applied.

Checking Leg Length and Stability
The hip is tested to ensure stability, correct positioning and equal leg length.

Closing the Wound
The layers are closed, usually with dissolvable sutures, and a dressing is applied.
Post-operative Treatments & Recovery
Recovery after hip replacement is an essential part of treatment. Most patients walk on the day of surgery or the morning after.
Pain Management
-
Modern techniques aim to reduce pain and speed up recovery.
This may include: - Spinal anaesthetic with light sedation
- Local anaesthetic injections
- Oral painkillers
- Ice therapy
- Many patients require only mild analgesics after the first few days.
Early Mobilisation
- A physiotherapist will guide you to:
- Stand and walk safely
- Use walking aids correctly
- Begin strengthening and stability exercises
- Early mobilisation reduces the risk of complications such as blood clots.
Physiotherapy and Rehabilitation
- Rehabilitation focuses on:
- Gait training
- Balance
- Strengthening the hip, gluteal and core muscles
- Regaining confidence and independence
- Recovery times vary, but many patients return to:
- Driving: 4–6 weeks
- Work (desk-based): 2–4 weeks
- Golf/cycling: 6–12 weeks
- Full activity: 3 months
Long-term Treatment After Knee Replacement
Continuing Strength & Mobility
- Patients benefit from regular low-impact activities such as:
- Walking
- Swimming
- Cycling
- Pilates
- These help maintain joint movement and reduce stiffness.
Protecting Your New Hip
- Avoid repetitive high-impact activities such as:
- Sprinting
- Long-distance running
- Jumping sports
- These increase the load on the implant and may shorten its lifespan.
Ongoing Review
- Follow-up appointments allow monitoring of:
- Wound healing
- Mobility and strength
- X-ray assessment
- Any signs of wear or loosening
- Most modern hip replacements last 15–20 years or more.
Risks and Complications
All procedures carry risks, although hip replacement is very safe. Potential complications include:
- Infection
- Blood clots
- Dislocation
- Leg length difference
- Fracture during surgery
- Nerve or blood vessel injury (rare)
- Wear or loosening over time
You will have the opportunity to discuss all risks and benefits in detail.