Knee Arthritis (Knee Osteoarthritis)
What is knee arthritis?
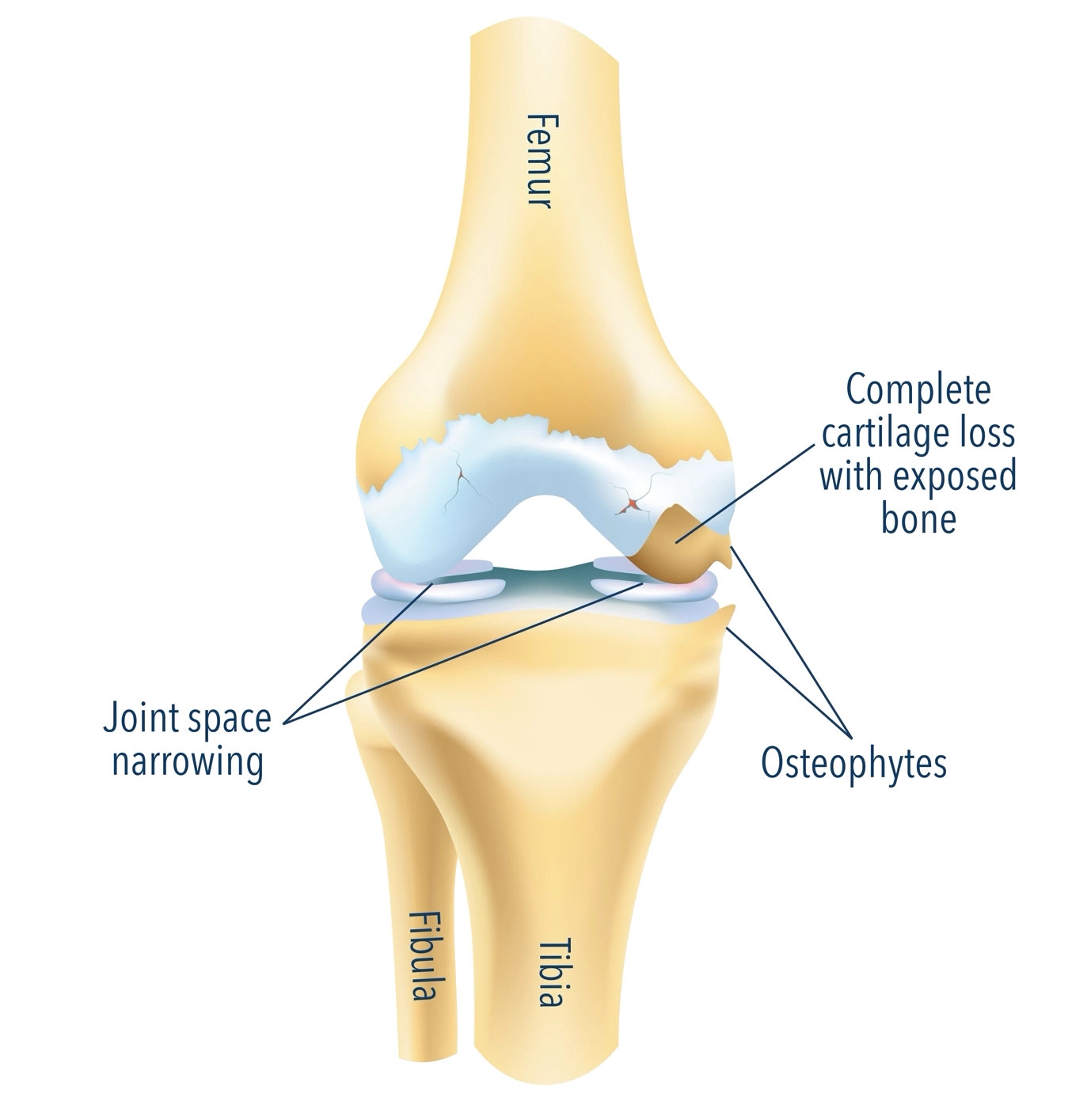
Knee arthritis—most commonly knee osteoarthritis—occurs when the smooth cartilage that lines the knee joint gradually wears away. Without this protective cushion, the bones rub together, causing pain, swelling and reduced movement.
The knee joint is formed of:
- The femur (thigh bone)
- The tibia (shin bone)
- The patella (kneecap)
All three areas may be affected by arthritis, and symptoms can vary widely depending on which parts of the knee are involved.
Knee osteoarthritis is extremely common and one of the leading causes of reduced mobility in adults.
Common symptoms
You may experience one or more of the following:
- Pain around the knee, often worse with activity
- Stiffness especially after sitting or resting
- Swelling
- Grinding, clicking or popping
- Reduced range of movement
- Difficulty with everyday activities:
-
- Climbing stairs
-
- Walking longer distances
-
- Squatting or kneeling
- Giving way or a feeling of instability
- Limping
Symptoms often develop gradually and can flare up after activity or changes in weather.
Why does knee arthritis occur?
Several factors contribute to the development of knee arthritis:
- Age-related wear and tear
- Previous knee injuries, such as meniscal tears or ligament injuries
- Malalignment of the leg (bow-legged or knock-kneed)
- A family history of osteoarthritis
- Excess body weight, increasing stress on the joints
- High-impact sports over many years
- Inflammatory conditions such as rheumatoid arthritis
Sometimes no specific cause is found.
Common symptoms
You may experience one or more of the following:
- Pain around the knee, often worse with activity
- Stiffness, especially after sitting or resting
- Swelling or a feeling of fullness
- Grinding, clicking or popping sensations
- Reduced range of movement
- Difficulty with everyday activities, including:
-
- Climbing stairs
-
- Walking longer distances
-
- Squatting or kneeling
- Giving way or a feeling of instability
- Limping
Symptoms often develop gradually and can flare up after activity or changes in weather.
Why does knee arthritis occur?
Several factors contribute to the development of knee arthritis:
- Age-related wear and tear
- Previous knee injuries, such as meniscal tears or ligament injuries
- Malalignment of the leg (bow-legged or knock-kneed)
- A family history of osteoarthritis
- Excess body weight, increasing stress on the joints
- High-impact sports over many years
- Inflammatory conditions such as rheumatoid arthritis
Sometimes no specific cause is found.
How is knee arthritis diagnosed?
Your symptoms, Daily activities and limitations, Previous injuries, operations or medical conditions
Walking pattern, Joint swelling or deformity, Tenderness, Range of movement, Ligament stability, Muscle strength
MRI may be requested if there is concern about a meniscal tear, ligament injury or other soft-tissue cause of pain
Together we will review your results and discuss treatment options tailored to your lifestyle and goals.
-
History :
We discuss:
Your symptoms, Daily activities and limitations, Previous injuries, operations or medical conditions -
Examination :
I will assess:
Walking pattern, Joint swelling or deformity, Tenderness, Range of movement, Ligament stability, Muscle strength -
Imaging :
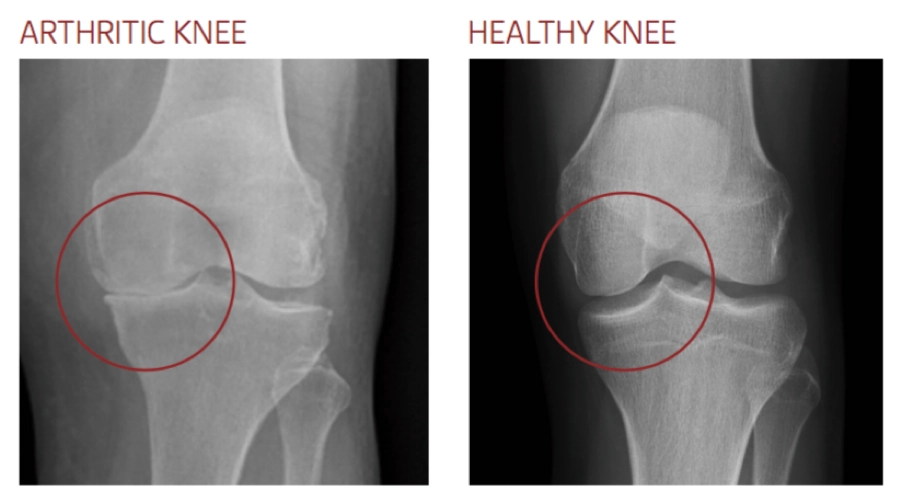
X-rays are usually sufficient to diagnose knee arthritis
MRI may be requested if there is concern about a meniscal tear, ligament injury or other soft-tissue cause of pain
Together we will review your results and discuss treatment options tailored to your lifestyle and goals.
History
We discuss:
- Your symptoms
- Daily activities and limitations
- Previous injuries, operations or medical conditions
Examination
I will assess:
- Walking pattern
- Joint swelling or deformity
- Tenderness
- Range of movement
- Ligament stability
- Muscle strength
Imaging
- X-rays are usually sufficient to diagnose knee arthritis
- MRI may be requested if there is concern about a meniscal tear, ligament injury or other soft-tissue cause of pain
Together we will review your results and discuss treatment options tailored to your lifestyle and goals.
Non-surgical treatment options
Many patients successfully manage knee arthritis without surgery for a long time. The following approaches can make a meaningful difference:
Exercise and physiotherapy
- Strengthening the muscles around the knee—especially the quadriceps, hamstrings and gluteal muscles—helps support the joint and reduce pain.
- Your physiotherapy plan may include:
- Strengthening
- Stretching
- Balance work
- Low-impact aerobic exercise (cycling, swimming, cross-trainer)
- Gait training
Weight management
Even small reductions in weight significantly reduce pressure through the knee joint—often easing pain and improving mobility.
Medications
- Paracetamol
- NSAIDs (such as ibuprofen or naproxen), if appropriate
- Topical anti-inflammatory gels
- Always follow your GP or pharmacist’s advice.
Braces, supports and lifestyle modifications
- Offloading braces may help in selected patients
- Using a walking stick on the opposite side
- Avoiding deep squatting or kneeling
- Choosing supportive footwear
Injections
- Injections may provide temporary relief by reducing inflammation or irritation:
- Steroid (corticosteroid) injections
- Viscosupplementation (hyaluronic acid) may be suitable for some patients
- Other injection therapies can be discussed case by case
- These can be useful as part of a broader treatment strategy.
When should surgery be considered?
Surgery becomes an option when:
- Pain significantly affects your quality of life
- Non-surgical treatments are no longer effective
- You struggle with mobility or sleep
- X-rays show moderate to severe arthritis
The main surgical treatments are partial knee replacement (in selected patients) and total knee replacement.
Partial Knee Replacement (Unicompartmental Knee Replacement)
- This may be suitable if arthritis affects only one part of the knee.
- Benefits:
- Smaller incision
- Quicker recovery
- More natural feeling knee
- Less blood loss
- Not all patients are candidates—this is based on examination and imaging.
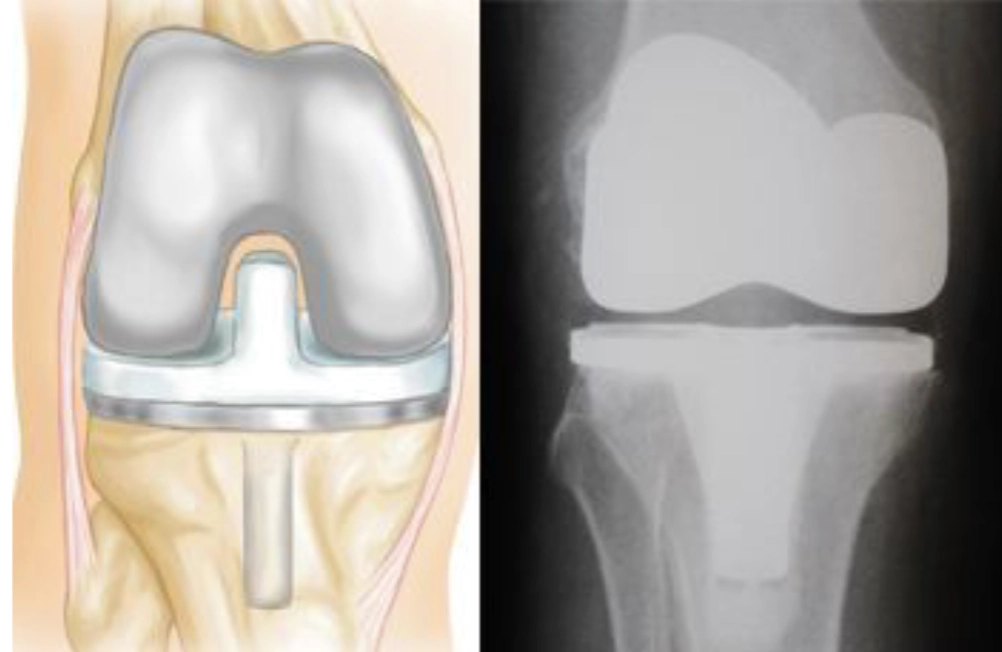
Total Knee Replacement
- A total knee replacement involves resurfacing the ends of the femur and tibia with smooth, metal-and-plastic components. The aim is to:
- Relieve pain
- Improve movement
- Restore quality of life
- Benefits:
- Most patients achieve:
-
- Significant pain relief
-
- Improved walking distance
-
- A straight, more stable knee
- Knee replacement surgery is highly successful and predictable, with excellent long-term results for the majority of patients.
Risks and complications
- Key risks include:
- Infection
- Blood clots
- Stiffness
- Persistent pain
- Implant wear or loosening over time
- Need for revision surgery
- We will discuss these in detail so you can make an informed decision.

Your journey with me
- Your knee care pathway typically includes:
- Initial consultation – history, exam and review of imaging
- Diagnosis and personalised plan
- Trial of non-surgical treatments
- Surgical discussion if symptoms persist
- Pre-operative planning
- Surgery (if needed) and early recovery support
- Post-operative follow-up and rehabilitation guidance
- My goal is to ensure you feel fully supported and informed at every step.
Frequently asked questions
Not necessarily. Surgery is based on symptoms and quality of life, not X-ray appearance alone.
Many modern implants last 15–20 years or more, depending on activity level and general health.
Most patients return to driving at 4–6 weeks, once safe to perform an emergency stop.
Some patients can kneel on a replaced knee, although it may feel uncomfortable. We can discuss your specific goals.
Yes—low-impact activities such as walking, cycling, swimming and golf are encouraged.