Hip Arthritis (Hip Osteoarthritis)
What is hip arthritis?
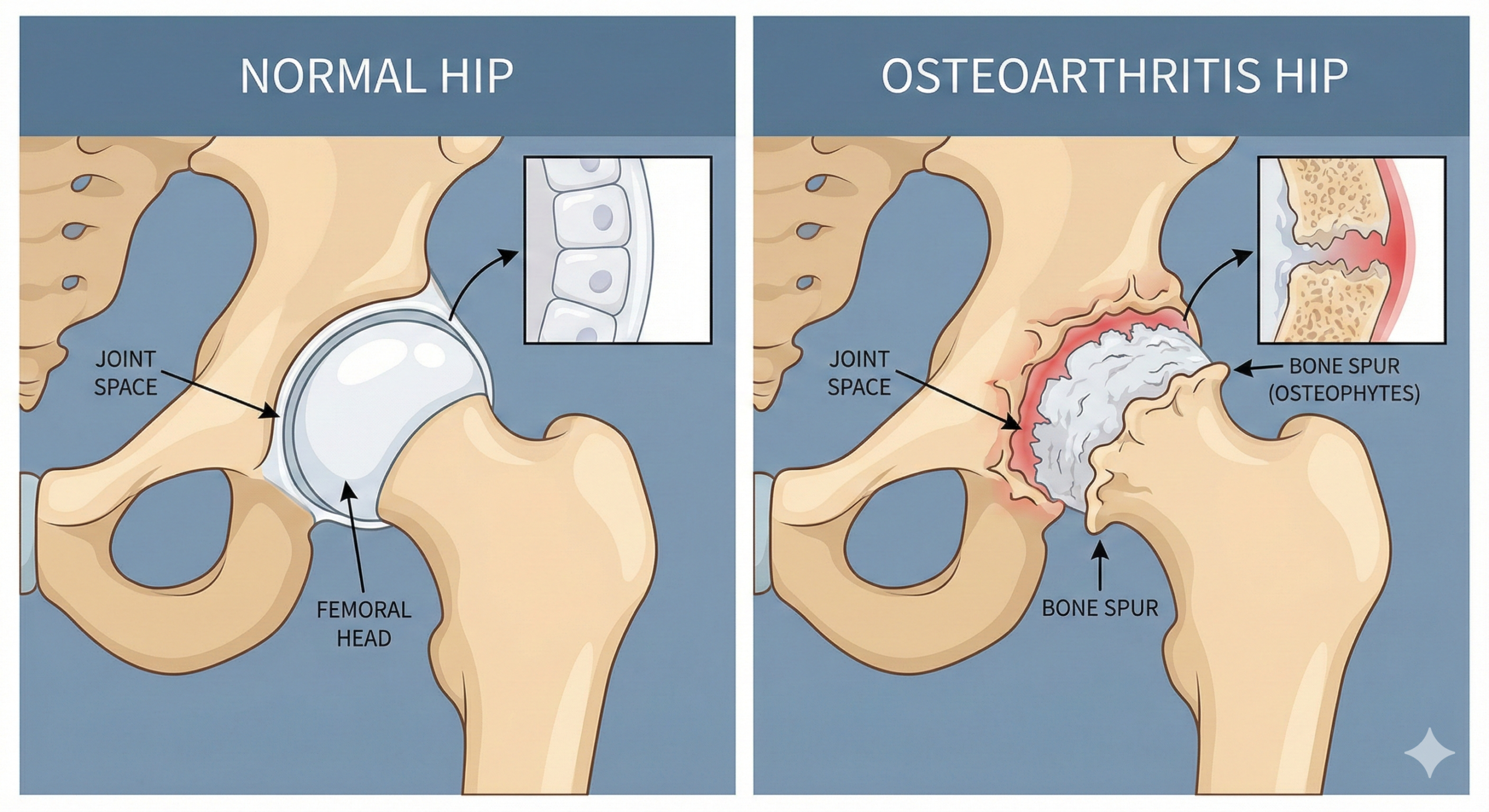
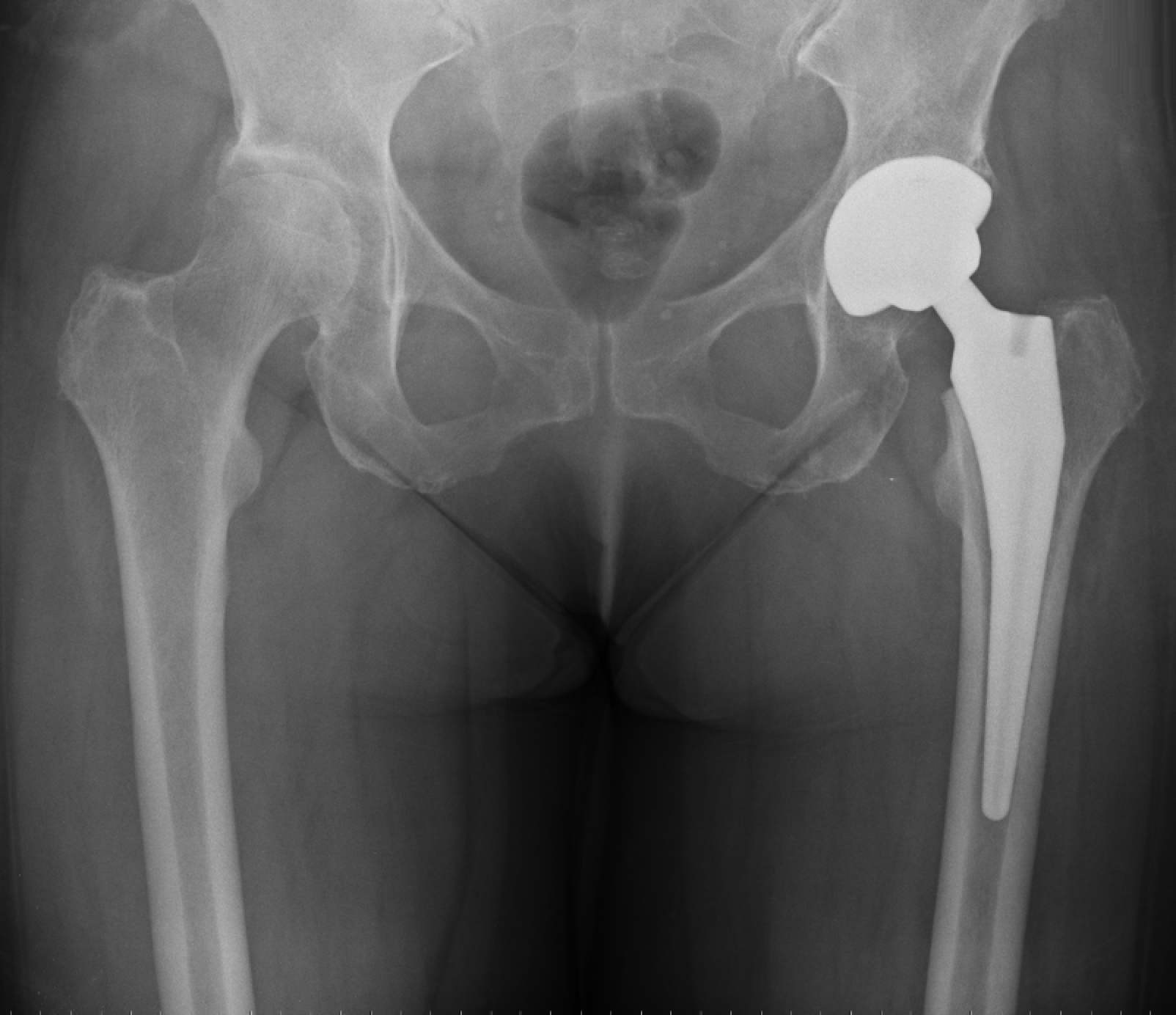
Hip arthritis (often called hip osteoarthritis) is a condition where the smooth cartilage lining the hip joint gradually wears away. The hip is a ball-and-socket joint: the ball is the top of the thigh bone (femoral head) and the socket is part of the pelvis (acetabulum). When the cartilage becomes thin or completely worn, the bones rub against each other, causing pain, stiffness and loss of movement.
Hip arthritis is very common and can affect people at any age, but is more frequent from mid-life onwards.
Common symptoms
Everyone experiences hip arthritis slightly differently, but typical symptoms include:
-
Groin pain:
Often felt deep in the groin, sometimes in the buttock or down the front of the thigh and knee -
Stiffness:
Particularly first thing in the morning or after sitting for a while - Pain when walking or standing for long periods
-
Difficulty with everyday tasks :
Putting on socks or shoes Getting in and out of a car Climbing stairs -
Reduced walking distance:
Needing to stop or rest sooner than you used to -
Limping:
Needing to use a stick for support - Clicking, catching or grinding
Groin pain
often felt deep in the groin, sometimes in the buttock or down the front of the thigh and knee
Stiffness
particularly first thing in the morning or after sitting for a while
Pain when walking
or standing for long periods
Difficulty with everyday tasks
such as:
- Putting on socks or shoes
- Getting in and out of a car
- Climbing stairs
Reduced walking distance
needing to stop or rest sooner than you used to
Limping
or needing to use a stick for support
Clicking, catching or grinding
sensations in the hip
Pain can start gradually and worsen over months or years, or it can sometimes come on more suddenly if there has been a flare-up or minor injury.
Why does hip arthritis happen?
In many people, hip arthritis is due to age-related wear and tear. However, there are several factors that can increase your risk:
- A family history of osteoarthritis
- Previous hip injury or fracture
- Childhood hip conditions (for example, hip dysplasia, Perthes’ disease or slipped upper femoral epiphysis)
- Being overweight, which increases the load on the joint
- Physically demanding work or high-impact sports over many years
- Inflammatory conditions such as rheumatoid arthritis
Sometimes there is no obvious single cause.
How is hip arthritis diagnosed?
→ Where the pain is and what it feels like
→ When it started and how it has changed
→ How it affects your day-to-day activities, work and hobbies
→ Any previous injuries, surgery or medical conditions
→ Your walking pattern (gait)
→ The range of movement of your hip
→ Areas of tenderness or muscle weakness
→ The spine and knee, as these can sometimes cause pain around the hip
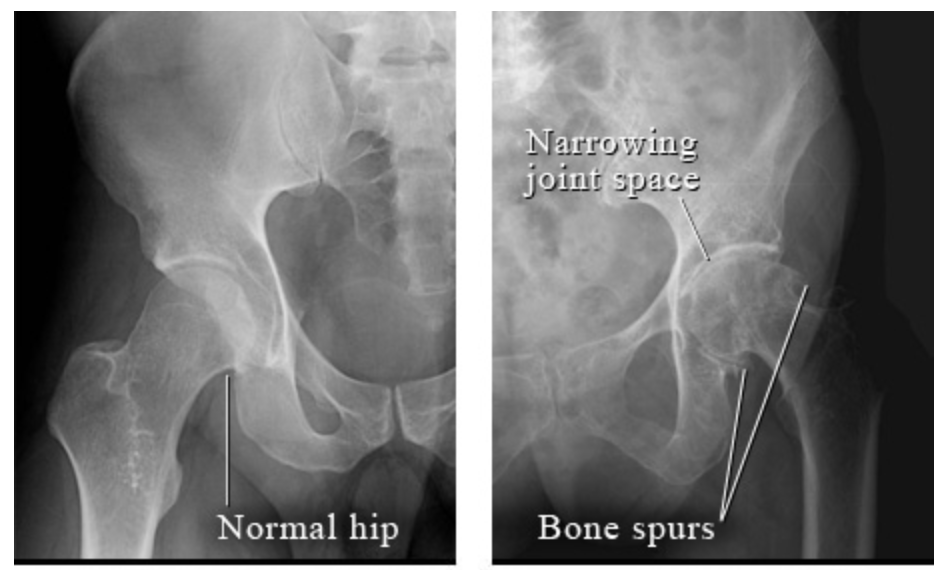
⚈ Narrowing of the joint space (loss of cartilage)
⚈ Bone spurs (osteophytes)
⚈ Changes in the shape of the ball or socket
→ Occasionally, an MRI scan or other tests are needed to rule out other causes of hip pain.
After this assessment, we can discuss the severity of your arthritis and which treatments are most appropriate for you.
Non-surgical (conservative) treatment options
Many patients can manage their symptoms for a long time without surgery. A combination of the following often works best:
Exercise and physiotherapy
- Strengthening the muscles around the hip, pelvis and core
- Stretching to maintain flexibility
- Low-impact exercise, such as cycling, swimming or cross-trainer
- Gait training and advice on posture and walking aids if needed
- The aim is to keep you as active and independent as possible.
Weight management
- If your weight is above the ideal range, even a small reduction can significantly reduce the load through the hip joint and improve symptoms.
Pain relief and anti-inflammatory medication
- Simple painkillers (e.g. paracetamol)
- Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen, if appropriate
- These should always be taken in line with advice from your GP or pharmacist, particularly if you have other medical conditions.
Walking aids and lifestyle adjustments
- Using a stick or walking pole in the opposite hand to the painful hip can offload the joint
- Avoiding long periods of standing or very high-impact activities
- Breaking longer walks into shorter, more manageable sections
Injections
- For some patients, image-guided injections into the hip joint can be helpful:
- Steroid injections can reduce inflammation and provide temporary pain relief
- In selected cases, other injection therapies may be discussed
- These are usually part of a wider treatment plan and are not a permanent cure.
Non-surgical (conservative) treatment options
Many patients can manage their symptoms for a long time without surgery. A combination of the following often works best:
Exercise and physiotherapy
- Strengthening the muscles around the hip, pelvis and core
- Stretching to maintain flexibility
- Low-impact exercise, such as cycling, swimming or cross-trainer
- Gait training and advice on posture and walking aids if needed
- The aim is to keep you as active and independent as possible.
Weight management
- If your weight is above the ideal range, even a small reduction can significantly reduce the load through the hip joint and improve symptoms.
Pain relief and anti-inflammatory medication
- Simple painkillers (e.g. paracetamol)
- Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen, if appropriate
- These should always be taken in line with advice from your GP or pharmacist, particularly if you have other medical conditions.
Walking aids and lifestyle adjustments
- Using a stick or walking pole in the opposite hand to the painful hip can offload the joint
- Avoiding long periods of standing or very high-impact activities
- Breaking longer walks into shorter, more manageable sections
Injections
- For some patients, image-guided injections into the hip joint can be helpful:
- Steroid injections can reduce inflammation and provide temporary pain relief
- In selected cases, other injection therapies may be discussed
- These are usually part of a wider treatment plan and are not a permanent cure.
Surgical treatment options
When should I consider surgery?
Surgery is usually considered when:
→ Pain is significantly affecting your quality of life
→ You are struggling with everyday activities despite non-surgical treatments
→ Pain is interfering with sleep, work or caring responsibilities
→ X-rays show moderate to severe arthritis
The most common operation for hip arthritis is a total hip replacement.
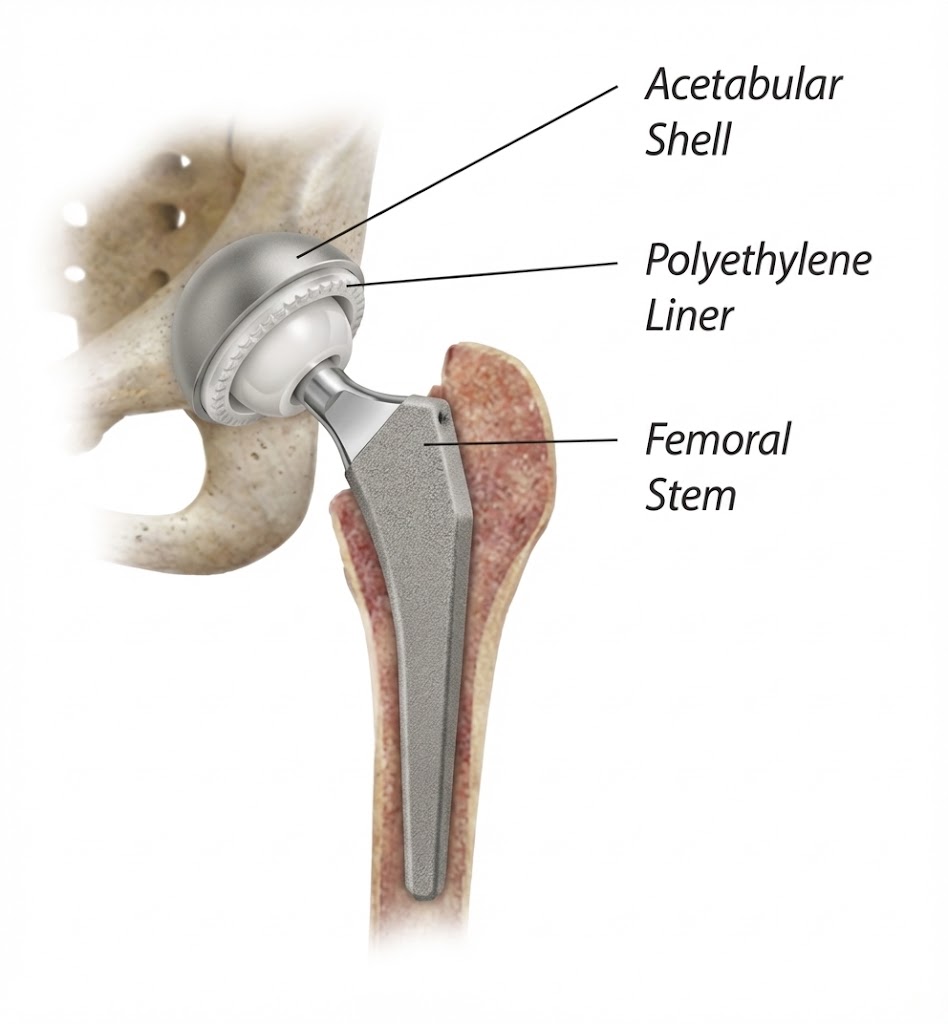
Total Hip Replacement
In a total hip replacement, the damaged ball and socket of the hip joint are removed and replaced with artificial components (a prosthesis). The aim is to:
→ Relieve pain
→ Restore movement
→ Improve your ability to walk and carry out everyday activities
Benefits
- Most patients experience:
- Significant or complete pain relief
- Improved walking distance and mobility
- Better sleep and ability to perform daily tasks
- A high level of satisfaction – hip replacement is one of the most successful operations in modern medicine
Risks and complications
- Any operation carries some risk. For hip replacement, the main risks include:
- Infection
- Blood clots (deep vein thrombosis or pulmonary embolism)
- Leg length difference or change in hip position
- Dislocation of the hip
- Wear of the components over time, which may eventually require revision surgery
- I will discuss these risks with you in detail and in the context of your individual health and activity goals.

Your journey with me
If you are referred or self-refer with hip pain, your pathway typically looks like this:
- Initial consultation – detailed history, examination and review of any existing scans
- Investigations – X-rays and, if necessary, further imaging
- Personalised treatment plan – starting with non-surgical options where appropriate
- Follow-up – to review your progress and adjust treatment
- Surgical planning – if needed, we will discuss the type of hip replacement, expected recovery and long-term outcomes
- Post-operative care – close follow-up after surgery, physiotherapy and return to activity guidance
Frequently asked questions
No. The decision is based on how much your hip is affecting your life, not just your X-ray. If pain and stiffness are stopping you doing the things you enjoy, it is reasonable to discuss surgery.
Modern hip replacements often last 15–20 years or more. Longevity depends on factors such as your age, activity level, bone quality and the type of implant used.
Most patients can return to driving after 4–6 weeks, once they are comfortable, walking safely and able to perform an emergency stop. I will advise you specifically at your follow-up.
Many patients return to:
- Walking longer distances
- Swimming and cycling
- Golf and similar low-impact sports
High-impact activities such as running and jumping sports are usually discouraged to protect the new joint.